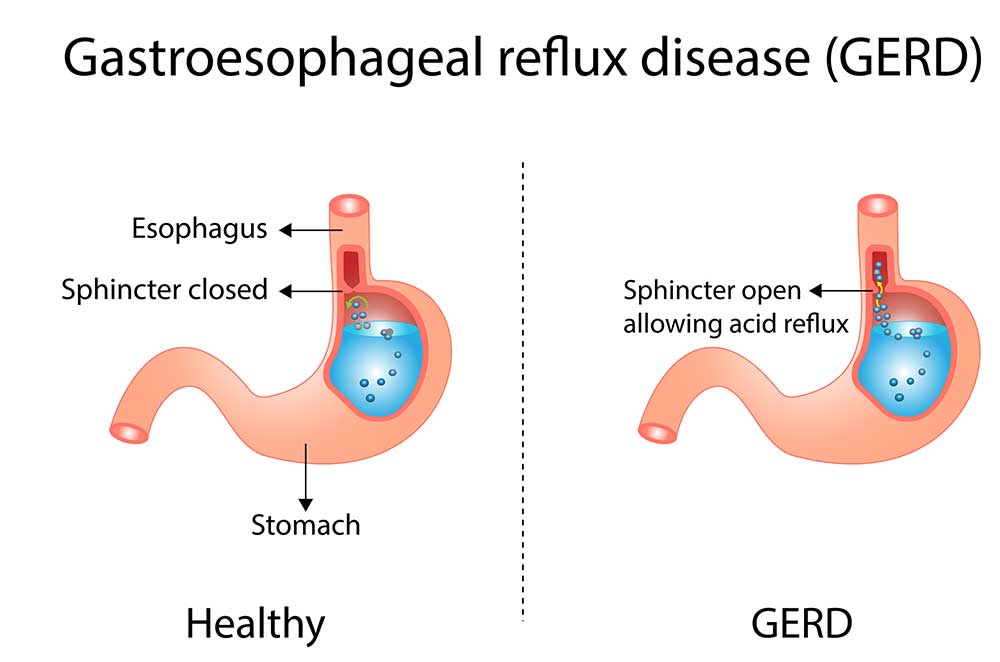
Severe heartburn, also known as gastroesophageal reflux disease (GERD), is a chronic condition that affects millions of people worldwide. It is characterized by a burning sensation in the chest and throat, and is caused by the backward flow of stomach acid into the esophagus.
Heartburn occurs when stomach acid frequently and persistently flows backward into the esophagus. This backward flow of acid irritates the lining of the esophagus, leading to the characteristic symptoms of heartburn, such as a burning sensation in the chest and throat.
Today, we will delve into the various symptoms of severe heartburn, including the causes, risk factors, diagnosis, and treatment options for heartburn.
Symptoms of Severe Heartburn
- Burning Sensation: One of the most common symptoms of severe heartburn is a burning sensation in the chest and throat. This burning pain, also known as acid indigestion or acid reflux, is often described as a sharp, stabbing pain that can be felt behind the breastbone and may worsen after eating or lying down. It is caused by the regurgitation of stomach acid into the esophagus, which irritates the lining of the esophagus and causes the burning sensation.
- Chest Pain: Severe heartburn can also cause chest pain, which is often mistaken for a heart attack. The chest pain associated with GERD is usually a dull, aching pain that may radiate to the back, neck, jaw, or arms. It may worsen with physical activity or stress, and may be accompanied by other symptoms such as shortness of breath, sweating, or nausea. It is important to differentiate between heartburn-related chest pain and chest pain due to a heart condition, as the treatment approaches may differ.
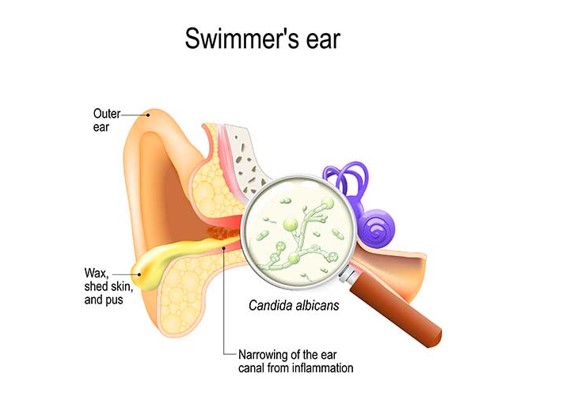
- Regurgitation: Another common symptom of severe heartburn is regurgitation, which is the sensation of stomach contents coming back up into the mouth. This can cause a bitter or sour taste in the mouth, and may be accompanied by the feeling of food or liquid coming up into the throat or mouth, especially when lying down or bending over. Regurgitation is caused by the relaxation of the lower esophageal sphincter (LES), a ring-like muscle that normally keeps the contents of the stomach from flowing back into the esophagus.
- Difficulty Swallowing: Severe heartburn can also cause difficulty swallowing, also known as dysphagia. This can manifest as a sensation of food getting stuck in the throat or chest, or as pain or discomfort when swallowing. Dysphagia may be caused by the inflammation and narrowing of the esophagus due to chronic acid reflux, and may require medical intervention.
- Chronic Cough: In some cases, severe heartburn can cause a chronic cough that persists even after other respiratory conditions have been ruled out. The cough may be dry or productive, and may worsen at night or after eating. It is believed that the irritation of the esophagus by stomach acid can trigger the cough reflex and lead to chronic cough.
- Hoarseness and Sore Throat: Severe heartburn can also cause hoarseness and sore throat. This is due to the irritation of the vocal cords and throat by stomach acid, which can lead to voice changes, hoarseness, and throat discomfort. These symptoms may persist despite usual treatments for a sore throat, such as lozenges or throat sprays.
- Dental Problems: Chronic exposure of the teeth to stomach acid due to severe heartburn can also lead to dental problems. The acid can erode the enamel, leading to tooth sensitivity, tooth decay, and gum problems. Dental issues may be an indication of long-standing GERD and should be evaluated by a healthcare professional.
- Asthma-like Symptoms: In some cases, severe heartburn can manifest as asthma-like symptoms, such as wheezing, shortness of breath, and chest tightness. This is known as reflux-induced asthma, and it is believed that the inhalation
Causes of Severe Heartburn
There are several causes of severe heartburn, and understanding them is crucial in order to effectively manage and treat this condition.
Here are the various causes of severe heartburn, including physiological, lifestyle, and other factors that contribute to its development.
- Dysfunction of the Lower Esophageal Sphincter (LES): The lower esophageal sphincter (LES) is a ring-like muscle located at the junction of the esophagus and the stomach. It acts as a barrier that normally prevents the contents of the stomach from flowing back into the esophagus. Dysfunction of the LES is a common cause of severe heartburn. When the LES fails to function properly, it may relax too frequently or not close tightly enough, allowing stomach acid to reflux into the esophagus, leading to heartburn. The exact causes of LES dysfunction are not fully understood, but certain factors, such as obesity, pregnancy, and hiatal hernia, can contribute to its weakening.
- Hiatal Hernia: A hiatal hernia is a condition where a portion of the stomach protrudes into the chest through an opening in the diaphragm, a muscle that separates the chest cavity from the abdominal cavity. Hiatal hernias can disrupt the normal functioning of the LES, leading to severe heartburn. The exact cause of hiatal hernias is not clear, but factors such as increased pressure in the abdomen due to obesity, pregnancy, or heavy lifting, weakened diaphragm muscles due to aging or injury, and congenital factors may contribute to their development.
- Diet and Eating Habits: Diet and eating habits play a significant role in the development of severe heartburn. Certain foods and beverages can trigger or exacerbate heartburn by relaxing the LES or increasing the production of stomach acid. Common dietary triggers of heartburn include acidic foods such as citrus fruits, tomatoes, and vinegar, spicy foods, fatty or fried foods, carbonated beverages, caffeine, chocolate, and alcohol. Eating large meals, lying down or going to bed immediately after a meal, and eating close to bedtime can also increase the risk of heartburn as they can cause stomach contents to reflux into the esophagus more easily.
- Obesity: Obesity is a significant risk factor for severe heartburn. Excess weight, especially around the abdomen, can increase pressure on the stomach and LES, leading to their dysfunction and resulting in heartburn. Additionally, obesity is associated with increased production of stomach acid, which can further contribute to the development of GERD. Losing weight through diet and exercise can help reduce the frequency and severity of heartburn in individuals with obesity.
- Pregnancy: Pregnancy is a common cause of heartburn in women. Hormonal changes during pregnancy, such as increased levels of progesterone, can relax the muscles, including the LES, leading to heartburn. Additionally, as the uterus expands, it puts pressure on the stomach, which can further contribute to the development of heartburn. Pregnant women should be aware of their increased risk of heartburn and take steps to manage it, such as eating smaller meals, avoiding trigger foods, and propping up the head of the bed while sleeping.
- Smoking: Smoking is a known risk factor for GERD and can worsen the symptoms of heartburn. Smoking weakens the LES and impairs its ability to function properly, leading to increased acid reflux into the esophagus.
Risk Factors of Severe Heartburn
While occasional heartburn is normal, persistent or severe heartburn can be a sign of a more serious condition and may require medical attention.
Here are the risk factors associated with severe heartburn.
- Diet: Diet plays a crucial role in heartburn. Consuming large meals, especially high-fat or spicy foods, can trigger heartburn in susceptible individuals. Foods that are acidic, such as citrus fruits, tomatoes, and vinegar, can also exacerbate heartburn. Additionally, carbonated beverages, caffeinated drinks, and alcohol are known to relax the lower esophageal sphincter (LES), the muscle that normally prevents stomach acid from flowing back up into the esophagus, leading to increased risk of heartburn.
- Obesity: Obesity is a significant risk factor for heartburn. Excess body weight puts pressure on the stomach, which can cause the LES to weaken, leading to increased acid reflux. Moreover, abdominal fat can compress the stomach, pushing acid up into the esophagus. Studies have shown that individuals with a higher body mass index (BMI) are more likely to experience heartburn, and weight loss has been associated with a reduction in heartburn symptoms.
- Pregnancy: Hormonal changes during pregnancy can relax the LES, leading to increased risk of heartburn. The growing uterus also puts pressure on the stomach, which can exacerbate acid reflux. Heartburn during pregnancy is common and usually resolves after childbirth, but it can be severe and persistent in some cases, requiring medical intervention.
- Smoking: Smoking is a well-established risk factor for heartburn. Nicotine, a chemical found in cigarettes, can weaken the LES and impair the normal functioning of the esophagus, leading to increased acid reflux. Smoking also increases the production of stomach acid, further contributing to heartburn. Quitting smoking is not only beneficial for heartburn, but also for overall health.
- Hiatal Hernia: A hiatal hernia is a condition in which a portion of the stomach protrudes into the chest through an opening in the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This can weaken the LES and disrupt the normal flow of stomach acid, leading to heartburn. Hiatal hernias can be congenital (present at birth) or acquired, and are more common in individuals over the age of 50.
- Medications: Certain medications can increase the risk of heartburn. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen, can irritate the lining of the esophagus and weaken the LES, leading to heartburn. Other medications, such as calcium channel blockers, nitrates, and sedatives, can also relax the LES and contribute to acid reflux.
- Medical Conditions: Several medical conditions can increase the risk of severe heartburn. Conditions such as gastroparesis (delayed emptying of the stomach), scleroderma (a connective tissue disorder), and achalasia (a condition that affects the function of the esophagus) can disrupt the normal movement of food and acid through the esophagus, leading to heartburn. Additionally, individuals with a history of peptic ulcers or gastroesophageal reflux disease (GERD) are at increased risk of severe heartburn.
- Genetics: Family history can also play a role in the development of heartburn.

Diagnosis of Severe Heartburn
The diagnosis of severe heartburn/GERD usually involves a combination of medical history, physical examination, and possibly additional tests.
- Medical History: Your healthcare provider will ask you about your symptoms, how long you have been experiencing them, and any factors that may trigger or worsen your symptoms. They may also ask about your medical history, including any past or current medical conditions that could be contributing to your symptoms.
- Physical Examination: Your healthcare provider may perform a physical examination, which may include listening to your heart and lungs, checking your abdomen for any tenderness or swelling, and examining your throat, mouth, and teeth.
- Endoscopy: An endoscopy is a procedure that involves using a thin, flexible tube with a light and camera (endoscope) to visualize the inside of the esophagus, stomach, and upper part of the small intestine. This can help your healthcare provider identify any abnormalities, such as inflammation, ulcers, or other changes indicative of GERD.
- pH monitoring: pH monitoring measures the level of acid in your esophagus over a period of time. This can help your healthcare provider determine the frequency and duration of acid reflux episodes and assess the severity of GERD.
- Imaging Tests: In some cases, imaging tests such as X-rays or a CT scan may be ordered to visualize the structure and function of the esophagus and stomach, and to rule out other conditions that may mimic severe heartburn/GERD.
- Trial of Medication: In some cases, your healthcare provider may prescribe medication to relieve your symptoms and may monitor your response to the medication as a way to confirm a diagnosis of GERD.
Severe Heartburn Treatment Options
If you’re experiencing severe heartburn, there are several treatment options available.
Medications
There are several types of medications that can be used to treat severe heartburn. These include:
- Antacids: Over-the-counter antacids like Maalox, Mylanta, and Tums can help neutralize stomach acid and provide temporary relief from heartburn.
- Proton Pump Inhibitors (PPIs): PPIs like omeprazole, lansoprazole, and esomeprazole are available by prescription and can reduce the production of stomach acid, providing longer-lasting relief from heartburn.
- H2 Blockers: H2 blockers like ranitidine, famotidine, and cimetidine can reduce the amount of acid produced by the stomach, providing relief from heartburn for several hours.
- Prokinetics: Prokinetic drugs like metoclopramide can help strengthen the lower esophageal sphincter (LES) and improve the movement of food through the digestive tract, reducing the frequency and severity of heartburn.
Lifestyle Changes
Certain lifestyle changes can help manage severe heartburn, including:
- Avoiding trigger foods and beverages: Spicy, fatty, fried, and acidic foods, as well as caffeine, alcohol, and carbonated beverages, can trigger heartburn in some people. Identifying and avoiding your trigger foods can help reduce heartburn symptoms.
- Eating smaller, more frequent meals: Eating smaller meals throughout the day instead of large meals can help prevent excess stomach pressure, which can contribute to heartburn.
- Avoiding lying down immediately after eating: Waiting at least 2-3 hours after a meal before lying down or going to bed can help prevent stomach acid from flowing back into the esophagus.
- Elevating the head of your bed: Raising the head of your bed by 6-8 inches can help prevent acid reflux during sleep by keeping your head and chest elevated.
Surgical interventions
In some cases, severe heartburn may require surgical intervention. These procedures are typically considered when medications and lifestyle changes have not provided adequate relief.
Surgical options for severe heartburn may include:
- Fundoplication: This is a surgical procedure that involves wrapping the top of the stomach around the lower esophagus to prevent acid reflux.
- Linx Device: The Linx device is a ring of tiny magnetic beads that is implanted around the lower esophagus to help keep the LES closed and prevent acid reflux.
- Endoscopic Procedures: Some minimally invasive endoscopic procedures, such as radiofrequency ablation (Stretta procedure) or fundoplasty, can be used to treat severe heartburn.
See a Board-certified ER Physician
It’s important to consult with a board-certified emergency room physician or other board-certified healthcare professional to determine the best treatment approach for your specific condition. They will consider the severity of your heartburn, your overall health, and other individual factors to develop a treatment plan tailored to your needs.